Measles (Rubeola)
Want help to write your Essay or Assignments? Click here
Abstract
Forty years after the licensing of an effective vaccine, measles continues to cause severe complications and death in children in the world. The most common complications from measles include pneumonia and encephalitis. Measles also remain a leading cause for blindness in the world. However, there has been some remarkable progress in the global measles program. In the past one decade, annual reports on measles have decreased by 77% that is from 146 per million populations to 33 cases per million people.
This is attributable to the wide coverage of safe and inexpensive vaccine. Nevertheless, there have been many incidences of measles outbreak in developed and developing countries. This is attributable to poor implementation of vaccination programs in developed and developing nations. This results to infection of 40 million people and results in 1 million deaths in the world.
Due to the highly infectious of the disease, a population immunity of 95% is needed in order to disrupt the transmission, but only a small fraction of the population gets vaccinated. In this regards, this paper explores the pathogen, the disease signs and symptoms, its transmission and preventive measures available. The paper will also explore the mechanism of measles vaccination in improving human immunogenicity.
Glossary
CDC: Centers for Disease Control and Prevention
CD8+: cluster of differentiation 8
CD4+: cluster of differentiation 4
CD46: cluster of differentiation 46
CD150: signaling lymphocyte activation molecule
CNS: Central Nervous System
EEG: electroencephalogram
pH: acidity or basicity of a substances
MV: Measles virus
SLAM+: Signaling lymphocytic activation molecule
SSPE: Subacute Sclerosing Panencephalitis
WHO: World Health Organization
Background
Measles is a viral disease that was first described by Rhazes- a Persian Physician in the 10th century. The incubation period and lifelong immunity after an infection was described by Peter Panum in 1846. The virus was isolated in 1954 in monkey and human kidney tissue by Enders and Peebles. The first measles vaccine was given license in the USA in 1963. Prior to the development if vaccine, the disease was nearly universal in early life stages, but most of the children would develop immune by the time they are 15 years.
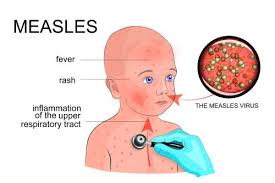
Although it is significantly managed in the USA, measles is still one of the major fatal diseases in the world. According to the World Health Organization (WHO), the disease causes 40 million infections with 1 million deaths globally in 2013. Measles is clinically manifested with cough, running nose, maculopapular rash, Koplik’s spots, low grade fever, and lymphadenopathy. In some cases, measles could lead to the infection of the respiratory tract or other organs including the skin, Kidney, bladder and viscera (Koehlmoos, Uddin, & Sarma, 2011).
Measles Virus
Measles is caused by a virus. This virus is known as Morbillivirus measles virus. It belongs to the family paramyxoviridae, order Mononegavirales and the genus Morbillivirus. The virus diameter is120-250 nm, and consists of single stranded RNA. The species is a close relative of canine distemper viruses and rinderpest.
There are two membranes that enclose the virus proteins. The membranes are responsible for the pathogenesis. The F (fusion) protein main role is to cause fusion of the virus to the host, haemolysis, viral infiltration; and Hemagglutinin (H protein) that causes the integration of the measles virus into the host cells. However, recent studies have reported changes in the H glycoprotein of the virus. Measles virus is inactivated by heat, acidic pH, trypsin and ether. Outside its host, the virus has a short life span which is normally less than 2 hours (Walsh, 2011).
The measles virus genome encodes 8 proteins, 6 structural proteins and 2 are responsible for viral entry. These are the Hemagglutin (H) as well as the measles virus fusion (F) protein. These proteins are the components of the viral envelope that together they mediate integration of the virus into the cells in the upper respiratory tract. The H protein targets the cellular receptors of the CD46 and CD150. This protein is is associated with the lifelong immunity that follows after recovery of the infection. This is attributable to the cell-mediated memory that causes the creation of neutralising antibodies that target the H protein of the measles virus (Walsh, 2011).
The measles virus life cycle starts with virus adsorption to host’s cell membranes surface using the H protein. The virus CD46 molecule is the cellular receptor. The virus then enters to the host cells where it uncoats. This is followed with RNA polymerase transcription of the Virus genome into the host mRNA. This is followed by the assembly of helical nucleocapsid occurs before the virus are released by budding. The mRNA synthesis, translation process and replication processes are as shown below (Walsh, 2011);
Want help to write your Essay or Assignments? Click here
Pathogenesis measles virus
The virus transmission is through droplet or airborne route. The nasopharynx is the primary infection site of the virus is the nasopharynx respiratory epithelium. The virus enters through the upper region of the respiratory system but the infection is not localized one specific site. The viral replication takes place in the epithelium of the respiratory system, and the replicated virons moves to lymphatic tissue.
Replication continues again in the lymph nodes and is from the lymphatic system that the virus spreads to the other different organs including the gastrointestinal tract, skin, and kidney. The virus replication takes places in the endothelial cells and epithelial cells of each of the aforementioned system. The virus has broad range of tissue tropism after it has accessed the epithelium (Walsh, 2011).
In each system, the virus replicates and sends it to the new virions which target the new host cells. The primary viremia is 2-3 days. After invasion, the virus replicates takes place in the respiratory epithelium and in lymph nodes as mentioned above. Following this replication, the second viremia takes place which is usually 5-7 days after initiation of the infection, which could lead to the infection of the respiratory tract or other organs including the skin, Kidney, bladder and viscera. The rash in measles and the Koplik’s spots arise from delayed hypersensitivity reaction (Walsh, 2011).
The pathogenicity of the virus takes place through in various distinct stages. The prodrome stage is the first stage. This stage is characterised by non-specific clinical manifestations such as fever, coryza, cough and conjunctivitis. However, addition signs and symptoms can be manifested during this prodrome stage. Small white spots can appear on the mucus membrane around the eye or sometimes along the parotid duct of the mouth. The spots are called the Koplik spots and precede the onset of skin rash. The Koplik spots are considered as diagnostic indicators, but are not present in all infections and also requires experienced healthcare provider to recognise them (Hanvoravongchai et al., 2011).
The onset of skin rash marks the end of prodrome. The rash is distinctive in that it is maculopapular and erythematous. The rash is attributable to immune reaction to endothelium and which occurs due to infiltration of mononuclear cells. The rash starts from the face and outspreads down to the trunk and lower extremities. The rash often lasts 3-4 days and dries up following a similar pattern. When the rash fades away, indicates that the viral clearance has begun. For uncomplicated incidences of measles, full recovery begins as soon as the skin rash begins to disappear (Guerrant, Walker, & Weller, 2006).
The third stage takes many forms and will occur where immunosuppression occurs and results to complications. When the patient is infected with measles virus, it induces immune response that is intense, which makes the host to be immunologically compromised. The reduction in CD4+ T helper cells, incapacitation of clonal activation of cell mediated and humoral immunity and reduction of CD8+ cytotoxic cells follows the viral clearance.
In addition, the antigen presenting capability is reduced due to maturation of then dendritic cells. The immunosuppression greatly affects the aspects of innate and adaptive immunity, and since the immunosuppression can last for sometime, the patient state of viral clearance makes them to become increasingly vulnerable. The immunosuppression can result to increased bacterial and viral infection. The most common type of infections is diarrhoea and pneumonia, which are responsible for increased paediatric mortality and morbidity associated with measles (Hanvoravongchai et al., 2011).
Measles virus has been isolated from the bronchial lymph nodes mononuclear cells and in tonsils in the first few days after infection Other studies have demonstrated massive infection in the lymph node, thymus and spleen. This suggests that it is possible that the virus primary target is the epithelial cells of the respiratory system and normally follow the SLAM + and CD46- independent pathway including the monocytes and lymphocytes.
The rash is occurs when T-cell reacts to the MV-infection in the capillary vessels. This is supported by the fact that the skin rash is absent from children with T-cell immunodeficiency. The mechanism that underlies the severe lymphonepia and immunosuppression is not well understood. However, the massive destruction of SLAM+ cells could cause the immunosuppression (Fields et al. 2013).
Acute measles panencephalitis normally involves the central nervous system (CNS). Transient EEG detects the brain abnormalities in 50% of the patient. It is difficult to isolate the measles virus from the patient’s brain. Therefore, the CNS damage arises from autoimmune reaction. The Subacute measles encephalitis occurs in patients with a history of severe immune disorder.
Therefore, the infections are not accompanied by production of antibodies. In SSPE, the virus gains entry to the CNS during the secondary viraemia. This causes a low grade infection that is persistent. It is not yet established if the lesions are due to immunopathological mechanisms or through viral replication (Walsh, 2011).
The human body immune system has a capacity to fight the measles viruses. The immune systems is carried out by specialized cells, each cell is designed to fight the disease. The microbe’s macrophages recognize the microbes through microbe’s specific antigen. The antigens trigger the lymph nodes to produce lymphocytes that are of two types- the T cells and B cells.
These cells are programmed by exposure to microbe’s antigen. The T cells function as defensive cells and offensive cells. The offensive cells work by attacking using chemotaxis. The defensive cells are the cytotoxic T cells also known as killer cells which usually identify the cells that are harbouring the microbes and release chemicals which destroy infected cells (Walsh, 2011).
The T helper cells help in activation of the T killer cells. The T helper cells works together with the B cells, which help secrete antibodies. The Antibody (Ab) that fights measles is produced and circulates in the blood system. The antibodies produced match the Ag sites for measles viral coat. The Abs then binds to the antigen in a specific matter. The Ab-Ag complexes have two effects.
First, the complex distorts the coat protein by attaching on its receptors. Secondly, the complexes have powerful chemical attractants of the white blood cells, which destroy the virus through phagocytosis. After viral clearance, the B cells and T cells are transformed into memory cells. These then quickly divide further into plasma cells making reserve antibody. In case of re-exposure to the measles virus, the immune system recognizes them and stops the infection. Through immunization, the live attenuated measles virus is injected in a person’s body.
The body responds by forming measles specific Abs through a process that mimics the actual infection of the virus. The viruses introduced are usually weakened and therefore cannot cause a disease, but it leads to formation of Memory cells. Thus, if the vaccinated persons get confronted with the real virus in the future, the body already have adequate quantity of anti-measles Abs, thus no infection results (Walsh, 2011).
Summary of an article
Eden and colleagues investigated the impact of novel microneedle measles vaccine in primates. The study hypothesised that use of microneedle patch will improve vaccination rates. The microneedle patches is a dry formulation of vaccines, which occurs in solid needles which dissolves upon application of the patch of microneedle puncture into the primate’s skin. The advantages of these patches are that they provide the opportunity of minimally-trained person to give the vaccination as there are no requirements for reconstitution. In addition, no single-dose presentation and avoids use of sharp waste, facilitates mass vaccination (Edens et al., 2015).
The microneedle vaccination systems are effective in delivering of vaccines. They have been effectively used in cotton rats, where the findings indicated that equal neutralizing antibody titers as those in cotton rats that had vaccination in subcutaneous injection. However, in this article, the animal model used is the rhesus macaques.
In this study, one group received live attenuated vaccine using microneedle patch and the other group using the subcutaneous injection. The serum samples collected were tested for presence antibodies, and the presence of IgM in day 14 after vaccination. The presence of IgM by day 14 is an indicator that the animal had generated immune response following immunization (Edens et al., 2015).
As shown in the Fig 1. , the neutralizing antibodies were detected at day 21 after vaccination, which accelerated and peek on day 28 in both groups. There was no statistical difference on the peak of titers and times to peak between the two groups. In subcutaneous injection and microneedle patch, the animals reached a titer higher than 120mlU/mL- which is normally considered as protective level in humans (Edens et al., 2015).
On matters concerning safety of microneedle patch vaccine, no side effects were observed. However, upon the removal of the patch, faint erythema was observed but there was no evidence of wound infection or bleeding. The faint puncture disappeared 2-3 days post vaccination and no swelling or discharge was observed. In addition, no reactogenicity or discomfort was observed.
This technique should be used in clinical practice as thermostability of the microneedle patches is considerably better as compared to the currently measles vaccine that are formulated and refrigerated during transport. Most of the vaccines denatures due to cold-chain failures (Edens et al., 2015).
Environmental factors that contribute to the re-emergence of measles and its impact in the society
The measles outbreaks have been hopscotching across the USA. It has not yet been confirmed on what exactly triggered the Disney linked measles outbreak, but the CDC officials have associated it with the overseas tourists who visit Disneyland Park. This is supported by the findings of genetic finger prints which was identical to B3 measles virus that had caused the massive measles outbreak in the Philippines. With the low vaccine coverage rate, the disease spread rapidly across the states. Medical professionals were quick to point to possibilities of anti-vaccine movement (Edens et al., 2015).
Research points out other contributing factors from public health measures such as lack of access to quality health care. For instance, surveys indicate that only 50% of pre-school aged children have been vaccinated against measles. Disparities in vaccination are observed in African American and Hispanic community. The vaccines for children program is for uninsured and medical eligible children.
The vaccine is give at no additional cost. However, still not every child gets immunized (Walsh, 2011). This is because some parents rejects vaccinations and another fraction may delay the child from getting immunization. This trend has increased in the recent past, which has resulted in unvaccinated communities. This poses a public health risk and barriers in achieving significant benchmarks for immunization coverage.
There are increased concerns that measles outbreaks have been reoccurring in areas that are least expected and in some cases in persons who have received vaccines in the past. This raises concerns on whether there is vaccine dilemma, or if the current vaccine must be insufficient and lacks adequate protective levels that will ensure that will enhance the circulation of measles specific neutralizing antibodies (Poland & Jacobson, 2012).
Measles have severe impact to the society. For instance, high measles fatality ratios have been reported in both developed and developing countries. In the developed countries, less than one in 1000 children diagnosed with measles dies. In developed country, measles is the leading cause of mortality in refugee camps. The risk of death depends on patient’s age, vitamin A deficiency, and malnutrition.
Most of the mortality is attributable to a number of measles complications such as encephalitis and pneumonia. The economic cost of the disease cannot be overlooked. CDC estimates that approximately $ 4,091-$ 10, 228 is used to contain each case of measles per day. The additional economic costs include the weighty costs of work absenteeism and children missing schools. These estimates indicates that the outbreak have a hefty price tag (Benjamin, 2014).
The resurgence of measles and most infectious disease globally reflects a quick fix mentality. There is poor development planning in infectious disease endemic regions, lack of institutional inertia and political determination. The re-emergence of infectious disease is inevitable because of high environmental and developmental change which results in increased population growth. There is much that can be done to reverse the current trend.
However, this will require meshing the economic and social developmental programmes with the natural resource and environmental programmes in order to establish strategic interventions that will reinvigorated the virus ecology and advancement of scientific measures. This will facilitate the strengthening of applied and basic research on the interaction of a pathogen, host and environment; which in turn will result in the development of vaccines, diagnostic procedures and new therapies required to detect and control the disease (Benjamin, 2014).
References
Benjamin Johns, D. (2014). Measles Eradication versus Measles Control: An Economic Analysis. J Vaccines Vaccin, 05(06). Retrieved from http://dx.doi.org/10.4172/2157-7560.s3-002
Edens, C., Collins, M., Goodson, J., Rota, P., & Prausnitz, M. (2015). A microneedle patch containing measles vaccine is immunogenic in non-human primates. Vaccine, 33(37), 4712-4718. Retrieved from http://dx.doi.org/10.1016/j.vaccine.2015.02.074
Fields, R., Dabbagh, A., Jain, M., & Sagar, K. (2013). Moving forward with strengthening routine immunization delivery as part of measles and rubella elimination activities. Vaccine, 31, B115-B121. Retrieved from http://dx.doi.org/10.1016/j.vaccine.2012.11.094
Guerrant, R., Walker, D., & Weller, P. (2006). Tropical infectious diseases. Philadelphia: Churchill Livingstone.
Hanvoravongchai, P., Mounier-Jack, S., Oliveira Cruz, V., Balabanova, D., Biellik, R., & Kitaw, Y. et al. (2011). Impact of Measles Elimination Activities on Immunization Services and Health Systems: Findings From Six Countries. Journal Of Infectious Diseases, 204(Supplement 1), S82-S89. Retrieved from http://dx.doi.org/10.1093/infdis/jir091
Koehlmoos, T., Uddin, J., & Sarma, H. (2011). Impact of Measles Eradication Activities on Routine Immunization Services and Health Systems in Bangladesh. Journal Of Infectious Diseases, 204(Supplement 1), S90-S97. Retrieved from http://dx.doi.org/10.1093/infdis/jir086
Poland, G. & Jacobson, R. (2012). The re-emergence of measles in developed countries: Time to develop the next-generation measles vaccines?. Vaccine, 30(2), 103-104. Retrieved from http://dx.doi.org/10.1016/j.vaccine.2011.11.085
Walsh, R. (2011). Measles Part 1: The Virus, the Disease, and the Dynamics. Retrieved from http://www.infectionlandscapes.org/2011/07/measles-part-1-virus-disease-and.html
Want help to write your Essay or Assignments? Click here