Want help to write your Essay or Assignments? Click here
Alzheimer’s disease
Since patient wandering and confusion are common for the patient with moderate-to-severe Alzheimer’s disease, what would the RN teach the family about maintaining a safe environment? Provide three examples.
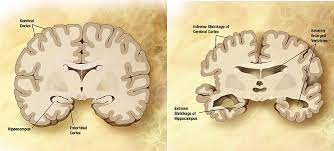
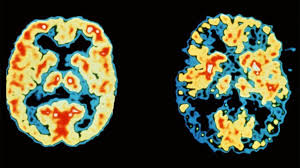
The RN should teach the family that patients diagnosed with Alzheimer can comfortably live in their homes, provided the safety measures are put in place. The family members must be educated on ways Alzheimer disease causes changes in the patient’s brain and body functions. This affects the patient reasoning, judgement, physical ability, behaviour, cognitive functions and sense of time (Bridenbaugh, Monsch & Kressig, 2012).
The family should be taught on ways to identify the possible dangers. The hazardous areas should be locked. Drugs and other chemical substances should be stored out of reach, in lockable cupboards. The family must be ready for emergencies. This implies that they should keep emergency phone numbers such as fire departments and local police helplines. The family members should ensure that the safety devices are working.
These include smoke detectors and carbon monoxide detectors and fire extinguishers. Walkways should be well lit to prevent falls. All weapons such as guns or other types of weapons must be removed. Basically, the home must be well lit, ventilated and free from hazards. The home should not be too restrictive, but one that encourage social interaction and independence (Schneider, 2011).
Want help to write your Essay or Assignments? Click here
To prevent the patient from wandering, the patient’s relatives and care givers should be taught the following strategies. To start with, they should create a daily activity plan. This helps identify the times of the day that wandering occurred. The patient must be reassured whenever they feel lost, disoriented or abandoned. The care giver must refrain from using correcting the patient using harsh voice.
All patients’ basic need must be met. They should not allow the patient to go places that trigger confusion and disorientation such as grocery stalls, malls or other venues that are busy. The doors must remain locked, and keys including car keys put out of sight. The patient must never be left alone i.e. they should always be under supervision. If the main issue is night wandering, devices that signal motions should be used (Lacey, Jones, Trigg & Niecko, 2012).
How would the RN adjust the teaching based on the family’s educational level, socioeconomic status or culture? Provide two examples
Despite the increase emphasis on patient centred care, when it comes to coping strategies for Alzheimer, the healthcare provider should focus on family centred care. In this case, the RN must conduct a family assessment to understand patient structure as well as style. This helps RN formulate effective teaching plan (Skoog, 2011).
To begin with, the RN should evaluate the barriers that would hinder the family ability to deliver health care. This includes the ages, sex and health status of the family member. The family socioeconomic status influences the teaching strategy. People from high socioeconomic status are most likely to be educated, thus basic healthcare can be used during the teaching process.
However, those from low income households tend to have low level of education which determines people’s attitudes and perceptions of care. Additionally, some family members lack basic knowledge of the disease. Cultural backgrounds could make some patients to believe in folk medicine. These factors must be addressed when teaching the patient’s family members (Trigg, Jones, Lacey & Niecko, 2012).
Want help to write your Essay or Assignments? Click here
What are common symptoms of caregiver role strain?
The demands of giving care to Alzheimer patients are very taxing which can lead to care givers strain and burnout. These are manifested through stress, anxiety, exhaustion, and sleep disturbances. Other common symptoms of care giver role strains include changes in appetite, depression, withdrawal and mood swings (Trigg, Jones, Lacey & Niecko, 2012).
Provide one nursing diagnosis statement (statement must include an actual nursing diagnosis, related factor and as evidenced by) that may be appropriate for a patient with moderate-to-severe Alzheimer’s disease.
Anxiety related to stress and situational crisis as evidenced by insomnia, restlessness, memory loss, and cognitive functions deficits.
References
Bridenbaugh, S., Monsch, A., & Kressig, R. (2012). How does gait change as cognitive decline progresses in the elderly?. Alzheimer’s & Dementia, 8(4), P131-P132. http://dx.doi.org/10.1016/j.jalz.2012.05.349
Lacey, L., Jones, R., Trigg, R., & Niecko, T. (2012). Caregiver burden as illness progresses in Alzheimer’s disease (AD): Association with patient dependence on others and other factors—Results from the Dependence in Alzheimer’s Disease in England (DADE) study. Alzheimer’s & Dementia, 8(4), P248-P249. http://dx.doi.org/10.1016/j.jalz.2012.05.660
Schneider, L. (2011). Agitation and Alzheimer’s disease. Alzheimer’s & Dementia, 7(4), S92. http://dx.doi.org/10.1016/j.jalz.2011.05.223
Skoog, I. (2011). Vascular Disease Risk Factors and Alzheimer’s Disease. Alzheimer’s & Dementia, 7(4), S284. http://dx.doi.org/10.1016/j.jalz.2011.05.822
Trigg, R., Jones, R., Lacey, L., & Niecko, T. (2012). Relationship between patient self-assessed and proxy-assessed quality of life (QoL) and patient dependence on others as illness progresses in Alzheimer’s disease: Results from the Dependence in Alzheimer’s Disease in England (DADE) study. Alzheimer’s & Dementia, 8(4), P250-P251. http://dx.doi.org/10.1016/j.jalz.2012.05.667
Want help to write your Essay or Assignments? Click here